General Surgery
CT-guided drainage of numerous abscesses
Acute bouts of appendicitis are the most common surgical emergency; unaddressed, serious complications will occur. This case will discuss the care for a ruptured appendicitis in a pediatric patient and how to properly diagnose appendicitis, thus preventing untoward outcomes.
Methods or Case Description:
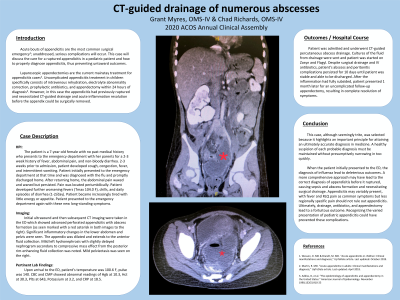
The patient is a 7-year-old female with no past medical history who presents to the emergency department with her parents for a 2-3 week history of fever, abdominal pain, and non-bloody diarrhea. Patient presented to the emergency department 3 weeks prior and was diagnosed with the flu and discharged. At home, the abdominal pain persisted until patient returned. CT and US imaging were taken in the ED after initial supportive treatment. CT imaging showed advanced perforated appendicitis with formation of numerous abscesses.
Outcomes:
Patient was admitted and underwent CT-guided percutaneous abscess drainage. Despite surgical drainage and IV antibiotics, patient’s abscess and peritonitis complications persisted for 10 days until patient was able to be discharged. After the inflammation had subsided, patient had an uncomplicated follow-up appendectomy, resulting in resolution of symptoms.
Conclusion:
When the patient initially presented to the ED, the diagnosis of influenza lead to deleterious outcomes. A more comprehensive approach may have lead to the correct diagnosis of appendicitis before it ruptured, causing sepsis and abscess formation and necessitating surgical intervention. Ultimately, drainage and appendectomy lead to the patient’s fortuitous outcome. Recognizing the varied presentation of pediatric appendicitis prevents these complications.
- GM
Grant Myres
Medical Student
Nova Southeastern University College of Osteopathic Medicine
SLC, UT, US - CR
Chad Richards
Nova Southeastern University College of Osteopathic Medicine
Davie, FL, US